CONDITIONS EXPLAINEDScoliosis
CONDITIONS EXPLAINEDScoliosis
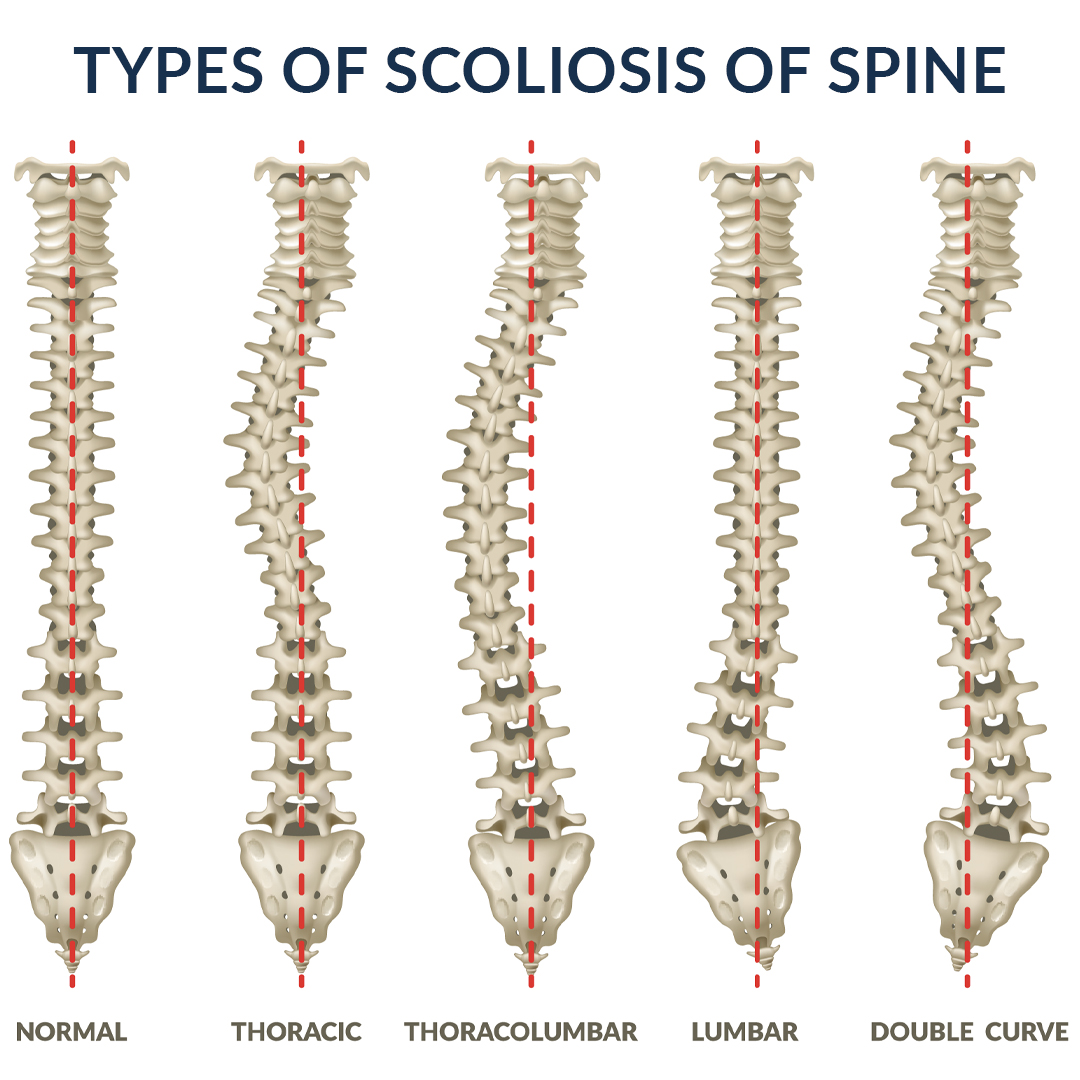
Scoliosis is a deceptively complex condition of the spine in which deformities occur in the curvature of the vertebral column. The visually apparent nature of scoliosis means frequent diagnoses in youth, and indeed is the most common spinal deformity in children. Though the degree varies between patients, the spine in scoliosis curves to either side forming an S shape. Presentation can range from a barely noticeable defect to life threatening breathing disruptions. Fortunately, most cases are fairly easy to treat with little more than consultation with a spine specialist and some orthopedic rehabilitation.
Physical changes are the most prominent feature of scoliosis, and asymmetries are usually clearly visible upon inspection. More serious symptoms may involve pain, radiculopathy, and loss of bowel and bladder control in the extreme cases. Prompt medical evaluation and treatment is essential to prevent unnecessarily permanent deformity.
Scoliosis is divided into several categories based on etiology and age of diagnosis. Most cases of scoliosis are diagnosed between the ages of 10 and 15. Idiopathic is a classification denoting an unknown cause, while scoliosis of known cause is named in relation to its etiology. Forms of scoliosis include:
- Infantile Idiopathic Scoliosis – Diagnosed between 0 and 3 years of age
- Juvenile Idiopathic Scoliosis – Diagnosed between 0 and 10 years of age
- Adolescent Idiopathic Scoliosis – Diagnosed between 11 and 18 years of age
- Congenital Scoliosis – Diagnosed from birth as a result of embryological anomalies
- Neuromuscular Scoliosis – May arise from brain, spinal cord, or muscular disorders, such as cerebral palsy or Arnold-Chiari malformations
- Syndromic Scoliosis – Occurs in conjunction with characteristic syndromes, such as Marfan’s
- Degenerative Scoliosis – Occurs when discs degenerate asymmetrically, shifting the supported vertebra to the side
- Thoracogenic Scoliosis – This form of scoliosis is secondary to medical procedures early in life such as radiation or surgery
Experiencing Symptoms of Scoliosis?
Detection & Diagnosis
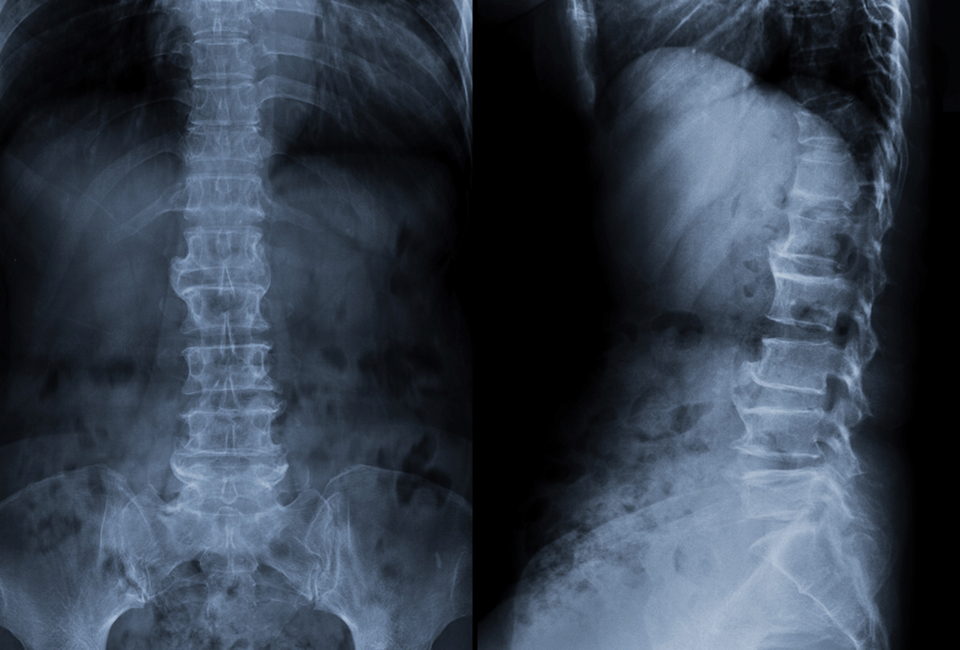
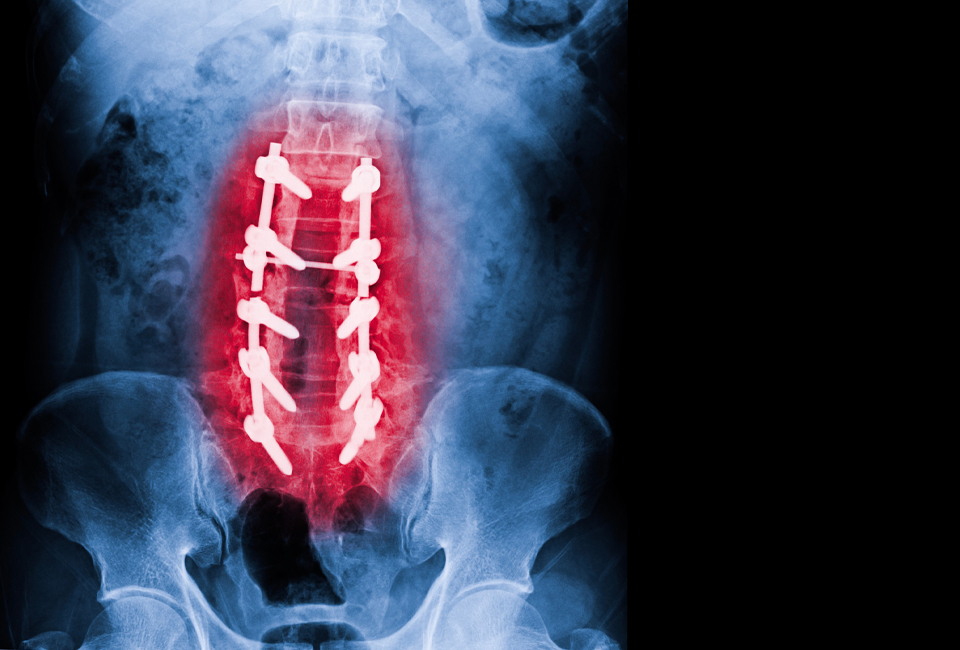
Screening for scoliosis is commonly performed for identifying the abnormality early. Physical examination aided by a scoliometer is typically adequate to identify the condition in most clinically relevant cases. For some patients, additional imaging studies may be ordered to visualize the spine and associated structures. These may include: